Introduction
Non-invasive ventilation (NIV) has been established since the end of the 1980’s as a treatment for chronic hypercap-nic respiratory insufficiency and has also asserted itself as an effective therapy option in neuromuscular diseases. If NIV is tolerated by the person concerned and if there are no distinctive bulbar symptoms with recurring aspirations, ventilation can be conducted with a mask [1]. At night an oronasal mask is preferred to prevent leakages via the mouth, but in the day a pure nasal mask is preferred to make talking or drinking easier as the ventilation continues. If there is an-other mask adequate for rest ventilation, for fluent speech but where respiratory capacity is no longer sufficient, inha-lation can also be supported intermittently by the ventilator through a mouthpiece. However, this often results in unde-sirable alarms [2]. This case report is intended to show that intermittent mouthpiece ventilation, offering good respira-tory support, can be established with the Vivo 50 without triggering disturbing alarms.
Case report
The person concerned, a 45-year old man, has been suffer-ing from amyotrophic lateral sclerosis (ALS), commencing peripherally, since 2007. During that time muscular weak-ness progressed to tetraplegia. The patient is still mobile using a special wheelchair. Because of hypercapnic respira-tory insufficiency with nocturnal pCO2 values of around 55 mmHg, non-invasive ventilation with a Vivo 50 and a mo-no-tube valve system over a full-face mask was initiated in January 2014. In May 2014 the person concerned used the ventilation for approximately 20-22 hours a day in the PSV(T-gV) mode, with an inspiratory pressure of 12 cmH2O and a PEEP of 0 cmH2O. Most of the time he was ventilated with a backup respiratory rate of 20/min. and with an inspiration time, Ti, of 1.2 secs. His inspiratory vital capacity, VCin, was still 0.52 litre. The person concerned complained of speech dyspnoea, he only had enough air for a maximum of 2 words and was highly dissatisfied with his ventilation situation. During the day he felt hyperventilated (pCO2 26.9 mmHg),
and could not talk very well under his full-face mask. He could not tolerate a nasal mask. In the nocturnal transcu-taneous CO2 and SpO2 measurement showed persistent hypercapnia of 55 (-60) mmHg and frequent desaturations. The presence of an assistant – primarily his wife – 24 hours a day was essential. A plane trip, which had been planned for some time to enable him to recover with his family, was put increasingly in doubt because of the unstable situation.
To improve the respiratory situation we used the feature on the Vivo 50 to set up different ventilation profiles: a ‘profile’ 1 for sleep by day and night with the aim of providing good ventilation and normalisation of the respiratory gases, and a ‘profile 2’ for activities during the day without disturbing hy-perventilation. For both profiles we opted for the PSV mode with a backup frequency of 18/min. and a target volume (TgV). In profile 1, with inspiratory pressures of 15-26 cm-H2O and a target volume of 650 ml. In so doing normal ven-tilation could be ensured both by night and day, at variable pressures, in order to achieve the target volume. Triggering of spontaneous breaths was also facilitated with moderate PEEP settings of 3 and 2 cm H2O respectively.
Moreover, in order to make talking easier, in particular, we selected, as a second gateway to ventilation, a mouthpiece with a flexible tube holder (“swan’s neck”) for securing to the table or wheelchair.
Contrary to the frequent practice of using an assisted vol-ume-controlled ventilation mode ,VCV(A) for mouthpiece ventilation [3], we decided to establish a third profile in the PSV mode with the following settings:
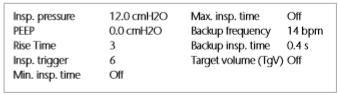
The settings of the backup respiratory rate and inspiration time were due to the fact that the Vivo 50 does not allow a backup respiratory rate below 4 breaths/min. and the back-up inspiration time cannot be set to zero. Although the ventilator discharges a brief blast of air from the mouthpiece every 4 seconds with the settings selected, this was not ex-perienced by the person concerned as disturbing and he was able to use the PSV mode with the mouthpiece inter-mittently to support his own breathing.
To prevent self-triggering of the respirator with the highly sensitively set inspiration trigger we also integrated an HME filter into the ventilating system in a patient-friendly manner. The person concerned was therefore able to trigger the de-sired breath without a problem at any time and without any disturbing false triggering.
Since a separate alarm management can be assigned to each ventilation profile with the Vivo 50 we were able to prevent all disturbing alarms by adapting the alarm limits to the mouthpiece ventilation (down to “low pressure” = 1.0 bar all alarms were switched to “off” for the mouthpiece ventilation). Since the person concerned was still capable of sufficient spontaneous respiration over an adequate period, close monitoring could be dispensed with.
Result
Thanks to the possibility of establishing two different pro-files for ventilation through the mask with the Vivo 50, the person concerned was now normocapnic at night and no further desaturations occurred. During the day he no lon-ger felt hyperventilated and was better able to trigger the ventilator. With the third ventilation profile set specifically for mouthpiece ventilation, he was able, when required, to trigger one or more breaths supported by the Vivo 50 fitted to the wheelchair with the flexible tube holder, which also enabled him to put together longer coherent sentences. As time progressed the person concerned learned to han-dle the mouthpiece ventilation well, and how to extend the times of use so much that a mask was no longer re-quired for ventilation during the day. His wife converted the Vivo 50 and changed the ventilation system for mouth-piece ventilation.
The person concerned can now be at home again without assistance for up to two hours (when he remains in contact with his wife via What’s App application on his mobile, he can continue working at the Home Office. He is mobile in his wheelchair throughout the day and his need for rest is
far less. He stresses that the adaptation of the Vivo 50 to his ventilation requirement, which changes during the course of the day, has considerably improved his quality of life and safety. Soon after his discharge from the hospital it was pos-sible to go on a planned holiday with his family. His flight travel while using mouthpiece ventilation on the Vivo 50 went smoothly, as did the entire holiday.
Conclusion
The possibility of setting different ventilation profiles on the Vivo 50 for this patient has made it possible to estab-lish mouthpiece ventilation in the pressure-supported mode PSV, in addition to differentiated and situation-specific ven-tilation through the mask, leading to a considerable subjec-tive improvement in the ventilation situation and enhanced quality of life and safety. Dyspnoea and the fear of situations causing dyspnoea have decreased and a high level of accep-tance of ventilation therapy has been achieved.
Abbreviations:
AF – Respiratory rate
ALS – Amyotrophic lateral sclerosis
EPAP – Expiratory Positive Airway Pressure
MPV – Mouth-Piece-Ventilation NIV – Non-invasive ventilation pCO2 – Carbon Dioxide Partial Pressure
PEEP – Positive End-Expiratory Pressure
TgV – Target Volume
SpO2 – Peripheral Oxygen Saturation VCin – Inspiratory Vital Capacity
Correspondence address:
Ingo Berweiler; Respiratory Therapist (DGP) ingo.berweiler@sana.de +49711-5533-21282
Bibliography:
[1] Windisch W. Walterspacher S, Siemon K. et al. Non-invasive and invasive ventilation as a therapy for chronic respiratory insufficiency – S2-Guideline, published by the German Association of Pneumology and Respiratory Medicine. Pneumologie 2010:64:207-240.
[2] Khirani S. Ramirez A, Delord V, et al. Evaluation of Ventilators for Mouth-piece Ventilation ion Neuromuscular Disease. Respir Care, September 2014 59:9 1329-1337
[3] Nicolini A, Russo D, Barlascini CO, Sclifo F, Grecchi B, Garuti GC, et al. Mouthpiece Ventilation in Patients with Neuromuscular Disease: A Brief
Clinical Review. Phys Med Rehabil Int. 2014;1(3): 1-4